There is an increasing body of evidence suggesting many of the components of cosmetic products, routinely applied, may have a negative impact on the tears and ocular surface and, in some cases, have been linked with more serious disease. In this review, our own Sarah Farrant, offers an overview of cosmetics, the risks they present.
Every now and again, I find myself confronted with a light bulb moment. In professional terms, this is
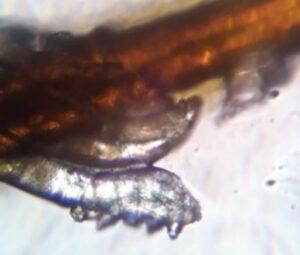
usually when it dawns on me that I have been completely underestimating something that I encounter regularly in clinic or with patients, but until that moment have not really spent any quality time speculating on the whys and wherefores. One such time in my career of great significance took place around 10 years ago when I first learned of the impact of Demodex spp and its influence upon the health of the ocular adnexa (figure 1). The can of worms (or mites in this case) that opened as I read that first CET article on the subject astounded me and, I can honestly say, my practice has never been the same since. Recently, I have experienced another such lightbulb moment.
WHY AN INTEREST IN COSMETICS IN EYE CARE PRACTICE?
As an optometrist and dry eye specialist, I have long since been aware, if only on a very superficial level, of the issues with cosmetics and make-up causing irritation to existing dry eye patients (myself included) and contact lens wearers resulting in poor tolerance or a flare in symptoms or both when eye make-up is applied. I have also seen numerous examples of caked layers of make-up on lids, pigment embedded in tarsal plates and floating debris in the tear films of determined wearers, enough to put you off your mid-morning chocolate chip cookie.
My general stance, until recently, was to offer standard general advice about inserting contact lenses before make-up application and ensuring all make-up was thoroughly removed at the end of each day, possibly forming part of a wider eyelid hygiene regime. In more recent years, I have also advised the use of lid hygiene products for blepharitis as a dual-purpose make-up remover. I did, however, stop short of telling patients to stop wearing make-up: That is like telling patients to stop wearing clothes. With no obvious alternative, it is definitely a non-starter. Besides which, I felt that a significant percentage of my dry eye patients were fairly self-selecting and ditched their make-up when it became too
much of a burden, able to recognise when it was clearly adding to their dry eye symptoms.
Looking further into our current understanding of the issues with standard make-up, what I have learned so far has genuinely shocked me. My aim for this article, therefore, is to outline the current issues, highlight what we know, and suggest what we should be considering on a daily basis when offering advice about cosmetic use by our patients.
FIRSTLY, WHY SHOULD WE EVEN CONSIDER COSMETICS?
Most of us have almost certainly not given cosmetics use in our patients much thought and are unlikely to be routinely asking questions during our consultations about patient’s current periocular cosmetic habits.
A recent study, however, highlighted that the prevalence of dry eye disease among women who used eye cosmetics was over 70%,
much higher than the 5 to 50% among the general population.
In addition, approximately 25% of participants using eye make-up rarely removed it before sleep. This was shown to be a further significant risk factor in the severity of dry eye. Given these figures, the impact of cosmetic products is something eye care practitioners cannot afford to ignore any more.

WHAT ARE COSMETICS?
Cosmetics come in all forms, though they are generally considered products that are rubbed, poured, sprinkled on, and or sprayed on the body and face to ‘beautify’ oneself. The use of cosmetics, by both men and women, has been around since ancient Egyptian times. Back then, cosmetics were used for a variety of reasons; to enhance beauty, to imitate the gods, for health, to protect the skin from the sun, and even to ward off evil spirits. Nowadays, the cosmetics that patients use on and around their eyes are not required to meet the same type of regulatory standards as ophthalmic pharmaceutical products, despite consisting of a wide range of chemicals, many of which are known not to be inert.
On average, women use 12 personal care products a day, exposing themselves to 168 chemical ingredients. Men use six, exposing themselves to 85 unique chemicals. The average age at which girls start to use cosmetics is around 12 years of age.
WHAT INGREDIENTS ARE IN COSMETICS?
As a practitioner, we encounter many different forms of agents and ingredients that we regularly recommend or prescribe to our patients, such as contact lens care solutions and ocular lubricants.
However, apart from the headline recognisable ingredients, I admit that most other constituents are a bit of mystery to me. This is yet more true for the ingredients of cosmetics. The list is usually so long, and in such small print, that it is a wonder that anyone ever bothers to read it (figure 2). The problem with this, to put it bluntly, is that they are not all safe to be used near the eyes.
This less than satisfactory situation has been allowed to continue, despite evidence of harmful effects from some constituents, because cosmetics lack the more stringent regulation required of medicines. As a result, certain ingredients in cosmetics and anti-ageing products have been identified as belonging to the following harmful classifications:
- Carcinogens
- Endocrine disruptors
- Neurotoxins
- Reproductive toxins
WHY DO COSMETICS IRRITATE DRY EYES?
Cosmetics and anti-ageing treatments used on and around the thin, and therefore easily penetrated, skin of the eyelids can, unfortunately, have an impact on the ocular surface. This impact may cause a number of adverse effects and may:
- Disrupt hormones
- Stress the ocular surface
- Increase the inflammation-inducing evaporative load of patients with ocular surface disease
- Irritate the cornea and conjunctiva
- Cause meibomian gland dysfunction and contribute to meibomian gland loss
- Contaminate the tear film
- Create tear film instability
- Promote demodex infestation
- Cause or exacerbate dry eye disease
Take, for example, benzalkonium chloride. This is a preservative and antimicrobial agent widely known among the eye care professions as an ingredient that causes insult to the ocular surface.
It is also authorised by the European Union for use in cosmetic products at maximum concentrations of 0.1% (1 mg/ml). This concentration is 20,000 times greater than that found to be toxic to human corneal, conjunctival and meibomian gland epithelial cells.
Other preservatives widely used in cosmetic products are formaldehyde (FA)-releasing compounds. According to Harvard Medical School research, the approved limit in cosmetics for FA-releasing compounds is some 740 to 2,000 times higher than the concentration shown to be toxic to human corneal, conjunctival and meibomian gland epithelial cells.
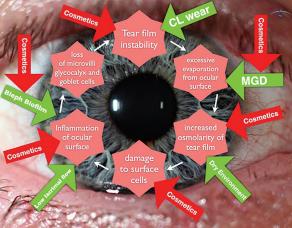
It is now accepted that dry eye disease persists and progresses as a vicious circle, one fuelled by a number of factors. Figure 3 shows various points of this circle where cosmetics can exacerbate the situation.
WHAT COSMETIC INGREDIENTS SHOULD WE ENCOURAGE PATIENTS TO AVOID?
It is way beyond the scope of this article to list all the chemicals in cosmetics that might be worth avoiding, and this list is ever-growing as further research into adverse effects is undertaken.
Interestingly, the US only bans 11 chemicals for use in the formulation of cosmetics, while the EU (and formerly the UK) bans more than 1,300. While this does make our job as eye care professionals rather difficult when patients ask for succinct and efficient advice, it is, at least, possible to provide information about some of the worst culprits. Table 1 lists 10 key ingredients to avoid (to see this you need to download the full document below), but remember that this is by no means an exhaustive list. It is worth noting the inclusion of terpinen-4-ol in this list, a key ingredient in many cosmetic tea tree oil-based products. It is also found in lid cleansers specifically designed to treat Demodex blepharitis as it has proved to be effective in killing demodex mites present on lash follicles. However, the ingredient has also been shown to cause a toxic effect on meibomian gland epithelial cells in vitro. 5,13, Because of this, it is always best to look at the overall risk-to-benefit ratio for any individual with a need to control their Demodex population, as well as to consider the appropriate minimum frequency and duration of use for each patient individually.
ANTI-AGEING AND ANTI-ACNE PRODUCTS
A significant number of anti-ageing products, and anti-acne creams, that are widely available in many countries contain retinol, also known as vitamin A or all-trans retinoic acid. Indeed, you may have some in your own bathroom cabinet at home. Retinol is obtained in the diet from plant or animal sources. Retinoic acid is the most active biological form of vitamin A while retinyl palmitate is the major storage form of vitamin A in the skin.
Retinol is found primarily in anti-wrinkle creams while another variant, called isotretinoin (13-cis-retinoic acid), is sold as Roaccutane; a common anti-acne cream. Retinoic acid is known to have a direct and significant damaging effect on meibomian glands. Indeed, it is not uncommon in my dry eye clinic to see younger patients who have been on isotretinoin to have significant gland loss at very young ages.

BAD HABITS
When we consider our own daily lives, most of us have many bad habits, perhaps more than we would ever want to admit in public, usually stemming from lack of time, ignorance or simply laziness. This is evident on a daily basis in my dry eye clinic, where patients frequently confess to practices that make my toes curl.
There are a number of typical bad habits to look out for regarding eye make-up use. These include:
- Sleeping in eye make-up
- Sharing eye make-up
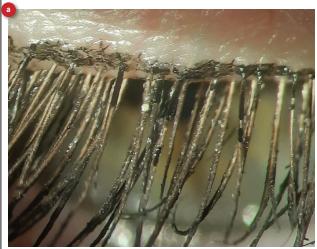
- Not replacing eye make-up regularly; mascara tubes can harbour a multiplicity of pathogens (figure 4). Many women keep their mascara for six to 12 months or more and, worse still, have been known to spit in the tube or add tap water to prolong use of the product.
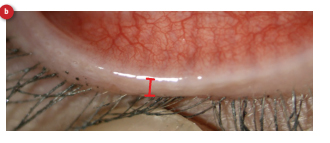
- Waterline (the inner eyelid margin) application of eyeliner
The term waterline is not a medical, anatomical label but a description coined by the fashion industry to describe the gap posterior to the eyelashes to the mucocutaneous junction along the lid margin at the point where the tears end and where the meibomian gland openings are to be found. Despite centuries of well-meaning advice to avoid using eyeliner along this zone, many wearers still persist in applying liner onto this area for some perceived improved cosmetic effect, whether real or otherwise.
The concern about doing so hinges upon the potential for cosmetic product to enter the tears and onto the ocular surface to cause an adverse response. A small but elegant study to verify the truth behind the risk of using eyeliner on the waterline was carried out by researchers from Cardiff and Waterloo Universities (19). The aim was to compare how much material from a conventional pencil eyeliner, applied to the periocular skin along one of two different locations, would subsequently migrate and contaminate the tear film. The two locations chosen were the waterline, the space behind the lash line, and the periorbital skin immediately anterior to the lash line (figure 5). The level of contamination was assessed by counting the number of glitter particles seen in the tears on slit lamp examination.
The results clearly supported the view that ‘eyeliner migrates most readily and maximally contaminates the tear film when applied posterior to the lash line.’ The study concluded that ‘it would be beneficial to advise patients to reserve the application of eyeliner pencils to anterior to the lash line. People who wear contact lenses are most likely to notice some problems. If they have eyeliner stuck to their lenses, increasing deposits might cause vision disruption as the lens becomes cloudier.’
It is worth directly addressing these common make-up misdemeanours.
CONTACT LENS WEAR AND COSMETICS
There is obviously a significant number of contact lens wearers who also wear make-up. Often the two modalities go hand-in-hand as there is a beauty enhancing element given over to both sides of this equation. As practitioners, we need to be aware that introducing make-up to a contact lens-wearing eye also carries with it some risk. Mascara and microplastics, such as the glitter in eyeshadow, can be both mechanically and chemically irritating if they flake into the tear film. These flakes can become trapped under soft or rigid corneal contact lenses. Pigments used in eye make-up might not be water-soluble and so can become lodged under a lens and potentially damage the ocular surface or cause corneal abrasions.

ARE PERMANENT COSMETIC ENHANCEMENTS BETTER THAN
DAILY COSMETIC PRODUCTS?
A not uncommon question from patients in my dry eye clinic is whether it is better to use more permanent or semi-permanent solutions instead of daily make-up. Such treatments include eye-
lash tinting, eyelash extensions or growth serums. The recent obsession on social media for extra-long lashes does not help in this regard.
FALSE LASHES
Sadly, this is another area of concern when it comes to ocular surface health. The adhesives used are cyanoacrylates, which adhere the false lash to the existing lash and often contain volatile
organic compounds and preservatives, such as formaldehyde.
Upon application, these chemicals can enter the eye and induce chemical conjunctivitis or keratitis. During wear, these products have been associated with contact dermatitis, allergic reactions
and inflammation, which may also exacerbate existing blepharitis. The other issue with false lashes is that patients may avoid proper lid cleaning for fear of dislodging the extensions. This also
adds to the ideal conditions for all manner of micro-organisms to establish.
EYELASH TINTING
Lash tinting is associated with severe conjunctival reactions and acute inflammation due to chemical toxicity as well as allergic response.
For advice for optometrists, case studies and references, please download the full article from CPD Optician below.
